Insulin Resistance, What You Really Should Know…
The Ins And Outs Of Insulin Resistance. How To Identify It, Symptoms Related To Insulin Resistance, Health Risks Associated With It And How To Fix It! Offering You More Than Just A Medication Option.
Insulin Resistance- The Buzz Word!
Insulin resistance seems to be a bit of a buzz word line item now, and it’s likely because it’s impacting more people than ever before here in America, even our kids. Previously it was pretty uncommon for individuals to have insulin resistance, struggle with weight concerns or have any subsequent findings of metabolic disease. Now insulin resistance is far more common to uncover. According to a 2015 study the presence of Type 2 Diabetes (developed over time) was present in about 9.8% of adults in the 1990s, as of 2012 about 12% of adults were diagnosed with Type 2 Diabetes and now estimates are about 15.8% of adults in 2023. What is perhaps more concerning is how diabetes is impacting our kids- in the span of 2001-2009 there was an increase of over 30% of youth being diagnosed with Type 2 Diabetes. So what does this really mean? Let’s break it down.
The Nitty Gritty On How This Works…
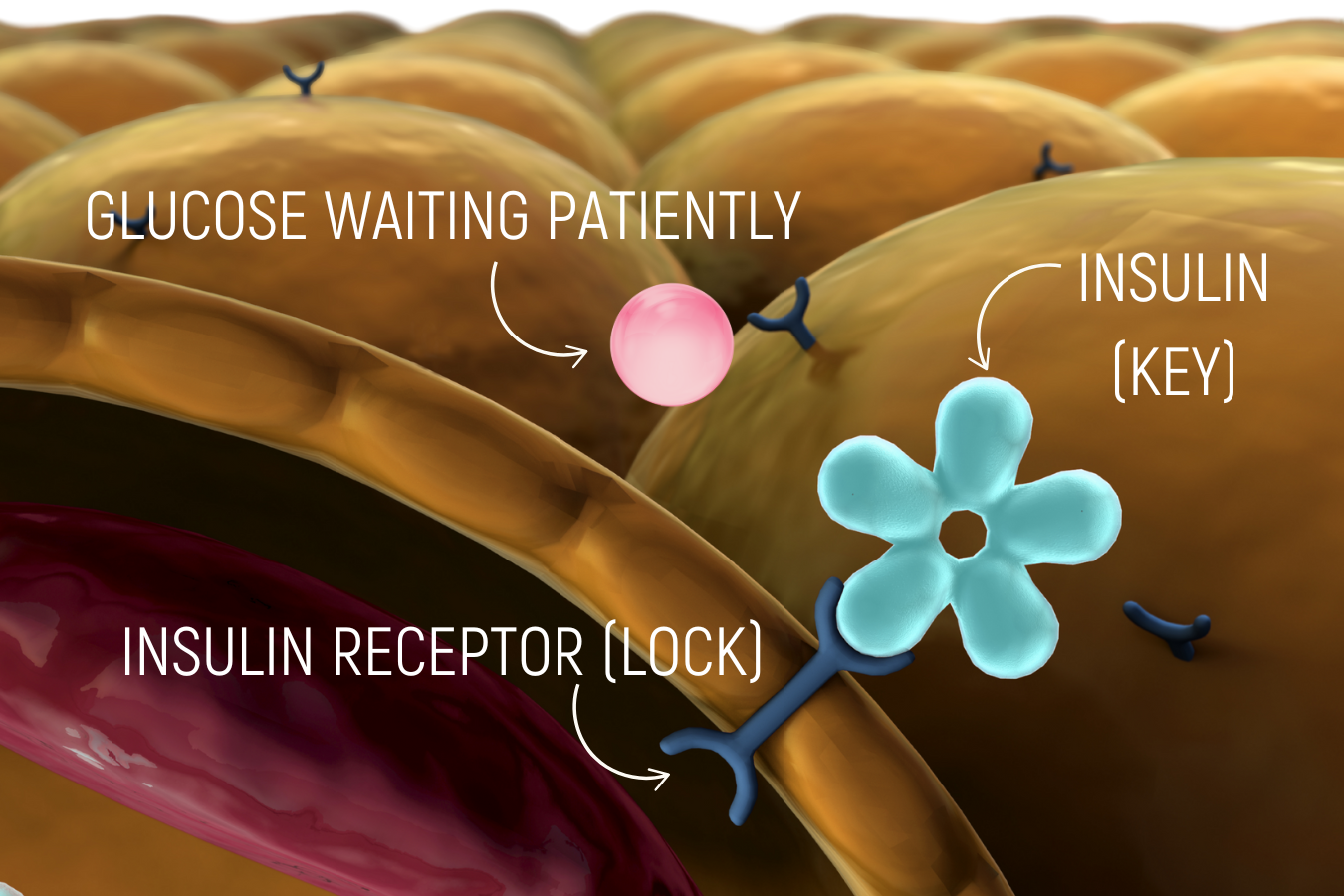
Glucose is the main sugar molecule on which our body operates and burns as fuel. We have more than just glucose in our food sources such as fructose for instance, but it, along with other sugar types are converted to glucose. Glucose is what we evaluate from a laboratory standpoint. When our system is working well we have glucose enter the body via food intake and find its way into the bloodstream. We then release insulin from our pancreas and in a lock-and-key mechanism, insulin opens the door to our cells to allow glucose to enter inside the cell from the bloodstream to then be used as fuel for energy.
When this goes awry, we have too much glucose too frequently so our cells start to think insulin sitting in the lock is just bluffing and we get less and less response. Our body can detect that glucose levels are not lower in the bloodstream so our intelligent cute bodies release more insulin which then goes and sits on those receptors on the cells. This means that beautiful lock and key mechanism breaks down and we then walk our way into insulin resistance. In a nutshell, our cells think we are bluffing and we require many locks to be filled, a secret password and a top secret handshake before we open the door to the cell to allow glucose inside.
How Do We Develop Insulin Resistance?
Okay so now that we understand what is going on, how the heck did we get here? There are a few ways we can overwhelm the system and land in insulin resistance. One way, which is blamed the vast majority of the time is food itself. Choosing the wrong types of food or simply being too high in our glucose/sugar intake and we swamp the system. If glucose is abundant all of the time or most of the time, our body is convinced we are simply “the boy who cried wolf” and you can huff and puff all you want, but we won’t open the door for glucose anymore, because this MUST be a trick! So our cells literally are less sensitive to that lock and key discussion.
A second way we can develop insulin resistance is stress. Yes, everyone’s most favorite. Whether it is mental/emotional stress or physical stress, our bodies will release stress hormones which make glucose (and fat cells) flood our system so we get a similar impact to the above. However, this results in a slightly different fashion than a food based issue. This type of insulin resistance happens with normal function at the level of the cellular signaling, we are simply overwhelming the system to gain the appearance of insulin resistance.
A third way to develop insulin resistance is through lifestyle choices. Physical inactivity promotes insulin resistance while more movement helps improve insulin sensitivity. This often is more related to how our body stores excess energy in the form of fat. When we store fat closer to our organs (visceral fat) we have higher risk of insulin resistance. This appears to be due to fat cells promoting more inflammation and breaking down the insulin-glucose conversation and opening the door to insulin resistance. Exercise, especially aerobic activity such as brisk walking and strength training can be particularly helpful in reducing and preventing visceral fat.
There Are Other Ways To Produce Insulin Resistance As Well But The Above Are The Primary Things We Need To Consider:
Food choices
Stress management
Lifestyle considerations to manage inflammation
Outside of those main drivers of the development of insulin resistance we also need to consider other disease processes that may also be taking place such as hypothyroidism, excessive cortisol levels (extreme cases are called Cushing’s syndrome), PCOS (polycystic ovarian syndrome), and certain medication use such as steroids.
So How Would We Even Know?
Symptoms of insulin resistance can be sneaky. Some of us can go without really detecting any symptoms at all. While others may be detecting energy crashes in their day related to blood sugar instability, skin tags on their body, darkening of the skin around the neck, armpits or groin, we can see weight gain, sometimes dullness in the right upper portion of the abdomen, anxiety and more.
This my friends, is where the beauty of ordering the correct testing comes into play. Most providers will order a hemoglobin A1c (HbA1c) which provides an estimation of blood sugar balance for the previous three months (ish). This is an actual calculation of how many red blood cells (RBCs) have become glycated (meaning a sugar shard has attached itself to the cell). The more sugar in the bloodstream the more “sugared-cells” we will see on the lab result. This is one way in which prediabetes or diabetes can be diagnosed. Normal ranges would be 5.6% and below, prediabetic findings would be 5.7-6.4% and diabetic findings are 6.5% and above.
Another format to formally diagnose prediabetes or diabetes is completing a fasting blood glucose. This is a standard component of screening labs within a “comprehensive metabolic panel.” A normal fasting glucose (meaning no food or drinks aside from plain water for 8+ hours) ranges between 70-99mg/dL. While a prediabetic fasting glucose result would be between 100-125 mg/dL and a diabetic finding would be 126 mg/dL or higher.
The third way to formally diagnose prediabetes or diabetes is through an oral glucose tolerance test (OGTT). If you have ever been pregnant you likely know exactly what this looks like; arrive fasting to your providers’ office, take a baseline blood draw, drink this super sugary drink (typically 50 grams of glucose), and wait. Blood is collected over the course of 1-3 hours (depending on the test). This is about as much fun as it sounds, so outside of pregnancy is not commonly utilized. Normal readings would be less than 140 mg/dL, prediabetic findings range 140- 199 mg/dL and diabetic findings exceed 200 mg/dL of glucose in the bloodstream after two hours.
A hugely under utilized test, and my personal favorite, is a fasting insulin assessment. Insulin, like we discussed above, is that super important hormone to encourage glucose into the cells out of the bloodstream. So when insulin is imbalanced it’s a fabulous way to detect issues before we have an abnormal fasting glucose finding or abnormal HbA1c (sometimes years ahead of time)! The range I am looking for and consider normal is between 2-7 microIU/mL. A study completed in2010 looked at 965 individuals, most of which were women (hooray) and found that individuals with fasting insulin of 4.9 (+/-1.2) microIU/mL showed best glucose management while those with fasting insulin 8.0 (+/- 0.8) microIU/mL and above had much higher risk of prediabetes/diabetes.
My favorite overall assessment of insulin resistance is utilizing a fasting glucose test and fasting insulin test taken from the same sample at the same time and calculating what is called a HOMA-IR. This is an acronym for Homeostatic Model Assessment for Insulin Resistance. In normal people terms- this is a predictive model of insulin resistance. It’s a simple calculation of fasting insulin and fasting glucose to provide the insight of likelihood of insulin resistance before we see signs of prediabetes or diabetes. This is one of my favorite tools to build a preventative plan of action!
What Options Do You Have To Manage Insulin Resistance?
So glad you asked! Fortunately we have many choices when it comes to how we want to combat insulin resistance. Our most powerful tools are the tools we use most often. You’ve guessed it, food choices and movement are the best. When it comes to the nitty gritty around food choices we can keep it broad or we can get really specific depending upon what works best for you. This is because, even with the best of intentions, if you cannot apply the plan, you will not get the results.
Broad Strokes Of Food Recommendations:
Reduce processed foods
Ditch soda, juice, energy drinks, alcohol, bougie coffees (aka- mocha frappucchino with 2 additional pumps of mocha sauce)
Ditch fast foods
Add all the fresh veggies, fruits and organic meats
Eat three meals per day consistently
High protein breakfast goal of 30g of protein or more
For those of us who strive with more concrete rules and advice one example I really like and see great outcomes with is The Whole30 diet. I have people utilize this as it was intended strictly for 30 days and then slowly open it up to find a place they feel comfortable with as a lifestyle change.
Movement is where we can see additional big strides in insulin resistance. We have some great longitudinal studies that show adults with insulin resistance who participate in regular physical activity can see a reduction in diabetes incidence by 58%. So I greatly encourage movement and I have individuals focus on strength training above aerobic exercise alone with a goal of 150 minutes of exercise per week. This shakes out to about 40-60 minutes of movement three times per week.
Herbal options are another way in which we can see benefits. I love to consider cooking with herbs such as cinnamon or garlic. Using tinctures or supplements that are rich in berberinecontent or even herbs like yerba mate. We also have mineral options to help improve blood sugar balance including chromium and vanadium. Sourcing and dosing minerals correctly is vital to good outcomes.
We have additional solutions such as balancing stress, improving sleep, reducing inflammation, managing other imbalances in the body and of course our standard approaches as well such as medications.
The point is, even if we find insulin resistance, you have an entire toolbox of options to get your body balanced again. If you don’t know where you stand from an glucose management standpoint and you’d like to know, or if you know you are managing insulin resistance, have a provider on your team to help discuss all of your options available to you and craft a plan that fits your personal needs! We are happy to see if we’d be a good fit for you, give us a call or sign up for an intro call and we will call you! Happy healing friends!